- Case Report
- Open access
- Published:
Tubal mesosalpinx cysts combined with adnexal torsion in adolescents: a report of two cases and review of the literature
BMC Pediatrics volume 24, Article number: 525 (2024)
Abstract
Background
Tubal mesosalpinx cysts are paratubal cysts, that account for approximately 10% of adnexal masses, and the presence of these cysts combined with adnexal torsion is a rare acute abdominal condition, with few cases reported in the literature. We reported two cases of adolescent tubal mesosalpinx cysts combined with adnexal torsion and reviewed the literature to help improve the diagnosis of the disease.
Case reports
The first patient was an 11-year-old girl with left lower abdominal pain for 5 days and fever with nausea and vomiting for 3 days, who was found to have a cystic pelvic mass on preoperative imaging and was diagnosed intraoperatively and postoperatively on pathology as having a left tubal mesosalpinx cyst combined with adnexal torsion. The second patient was a 13-year-old girl with right lower abdominal pain for 16 h and a palpable mass in the lower and middle abdomen on examination, which was hard and tender to palpate. Preoperative imaging revealed a large cystic mass in the right adnexal region, and intraoperative and postoperative pathology revealed a right tubal mesosalpinx cyst combined with adnexal torsion.
Conclusions
Tubal mesosalpinx cysts combined with adnexal torsion are rare causes of acute lower abdominal pain. Early diagnosis and timely surgery are necessary to ensure ovarian and tubal function. Accurate preoperative imaging diagnosis is challenging, and MRI is a beneficial supplement to ultrasound and CT examinations, providing more objective imaging information and reducing the incidence of adverse outcomes.
Background
Tubal mesosalpinx cysts are paratubal cysts, that mostly occur in women of childbearing age and are rare in children and adolescent women [1]. It may lead to acute complications, such as rare adnexal torsion, which is more difficult to diagnose preoperatively. Adnexal torsion is the twisting of the adnexa around the infundibulopelvic ligament and the ovarian ligament. It is one of the gynecological acute abdominal conditions [2, 3]. Adnexal torsion carries certain risks to future fertility, so early diagnosis and immediate intervention are necessary to ensure ovarian and tubal function in young female patients with adnexal torsion. However, due to the lack of specificity of its clinical manifestations, preoperative diagnosis of this disease is extremely difficult and it is often misdiagnosed, leading to delayed treatment [4]. We reported two cases of adolescent girls who were diagnosed with tubal mesosalpinx cysts combined with adnexal torsion and reviewed the literature to help improve the diagnosis of the disease.
Case reports
Case 1
An 11-year-old girl was admitted to the hospital with “left lower abdominal pain for 5 days and fever with nausea and vomiting for 3 days”. On physical examination, the abdomen appeared flat, the abdominal wall was soft, and there was tenderness and rebound pain in the left lower abdomen. Laboratory examination revealed a leukocyte count of 1.8 × 104/L with no other abnormalities. The adolescent had her menarche half a month ago and experienced no menstrual pain.
Ultrasound revealed a cystic echo approximately 6.88cmx5.03 cm in the left adnexal region, with clear borders and regular morphology, and an enlarged and twisted ovary in front of the lesion on the same side, which is closely related to the cystic lesion, and the “ovarian crescent sign” [5] can be seen. CDFI showed no blood flow signal(Fig. 1a). CT revealed a cystic lesion on the left side of the pelvis, measuring approximately 6.80 cm x 5.07 cm with a CT value of roughly 10 HU (Fig. 1b and c). On MRI, the lesion displayed a low signal on T1WI and a high signal on T2WI. The boundary between the lesion and the left ovary was unclear. The left ovary exhibited swollen morphology and uneven density. The uterus showed external compressive changes and had a clear boundary with the cystic lesion (Fig. 1d).
Imaging examination. (a) Ultrasound revealed a cystic echo (short arrow), poorly demarcated from the left ovary (slender arrow). (b and c) CT showed a round-like cystic lesion (short arrow) closely related to the left ovary (slender arrow), and the uterus (yellow arrow) showed extrinsic compressive changes. (d) The MRI sagittal view showed a round-like high signal (short arrow), and the lesion was poorly demarcated from the left ovary (slender arrow)
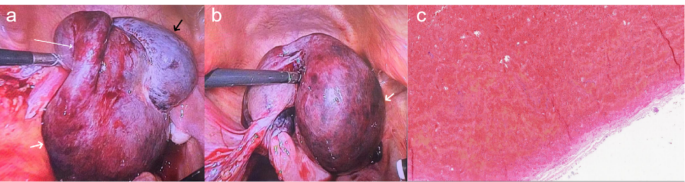
Surgery: Laparoscopic surgery was performed under general anesthesia. Intraoperatively, two trocars are placed lateral to the left rectus abdomins muscles, 2 cm above and 2 cm medial to the anterior superior iliac spine, respectively. Then, another trocar was placed at the right reverse McBurney’s point. It was found that the left adnexa was significantly enlarged with purplish-blue ischemic changes, and a cyst with a diameter of approximately 8 cm was observed in the left tubal tract area. The left fallopian tube and ovary twisted 2 turns along the infundibulopelvic ligament (Fig. 2a and b). We repositioned the left adnexa, restored its blood supply. The ovary and the cyst were completely separated, and the cyst was completely stripped.
Operative findings during laparoscopy and postoperative pathological microscopic findings. (a and b) The left ovary appeared enlarged and purplish-blue (black arrow). The left fallopian tube (slender arrow) and ovary (black arrow) twisted 2 turns along the pelvic funnel ligament. A mesenteric cyst (short arrow) was observed adjacent to the left fallopian tube. (c) Postoperative pathological microscopic findings
Postoperative pathological microscopic findings: The specimen exhibited cystic wall-like tissue without clear overlying epithelium and significant hemorrhage within the wall, consistent with a cyst (Fig. 2c).
Case 2
A 13-year-old girl was admitted to the hospital with a complaint of “16 hours of pain in the lower right abdomen.” On physical examination, there was tenderness and rebound pain in the lower right abdomen, along with the detection of a mass measuring approximately 15.00 cm x 12.00 cm in the middle and lower abdomen. The mass exhibited a hard texture, tenderness, and mobility. The adolescent had her menarche one year ago and experienced no menstrual pain.
Ultrasound revealed a large cystic mass measuring approximately 16.00 cm x 10.00 cm in the right adnexal region, which was well demarcated from the ovary, and the ovarian crescent sign was visible. Torsion of the ovary secondary to pulling by the lesion. An enlarged ischemic right ovary measuring approximately 8.40 cm x 3.80 cm was detected next to the twisted tip, with no clear blood flow signal.
CT revealed a giant cystic occupancy on the right side of the pelvis, measuring approximately 16.50 cm x 11.84 cm. The fluid in the capsule was uniform in density, with a CT value of approximately 4 HU, and the wall of the capsule was slightly hyperdense. Its upper border extended to the lower border of the liver, and its lower border adjoined the right ovary and the right horn of the uterus. The uterus was shifted to the right side. The boundary between the cyst and the ovary was still clear, and there was a close local relationship. In addition, it can be observed that the right fallopian tube has thickened and twisted (Fig. 3a and b, and 3c).
(a)The CT coronal view showed a large cystic mass (slender arrow) in the pelvis, whose upper border reached the inferior border of the liver. (b)The lower border of the large mass (slender arrow) pulled the right ovary (short arrow) and the right horn of the uterus (bold arrow). (c)The CT sagittal view showed the lower edge of the large mass (slender arrow) pulled the ovary (short arrow), causing it to deform and shift. (d) Postoperative pathological microscopic findings
Surgery: Laparoscopic surgery was performed under general anesthesia. Intraoperatively, the pneumoperitoneum was first estalished. Two trocars were placed lateral to the left rectus abdomins muscles, 2 cm above and 2 cm medial to the anterior superior iliac spine, respectively. A drainage needle was used to extract some of the cystic fluid to reduce the volume of the cyst and facilitate subsequent operations. Then, another trocar was placed at the right reverse McBurney’s point. Laparoscopy showed the cyst originated from the right tubal mesosalpinx, approximately 16 cm in diameter. The cyst, together with the right adnexa, was twisted for 2 turns along the infundibulopelvic ligament. The right ovary was ischemic and swollen, with a purplish-blue color, and the right adnexa was reset to restore its blood supply. The ovary and the cyst were completely separated. Then, the cyst was completely stripped away.
Postoperative pathological microscopic findings: The specimen showed a fibrous tissue capsule wall, lined with columnar epithelium, vascular dilatation and congestion, and plasma exudation in the capsule (Fig. 3d).
Discussion
Tubal mesosalpinx cysts are independent of the fallopian tubes and ovaries. They originate from the broad ligament between the fallopian tube and the ovary and are easily confused with cystic masses originating from the ovary. They are histologically derived mainly from mesonephric duct remnant tissue, and their pathologic types include paratubal cysts, mesonephric duct cysts, and mesothelial cysts [6, 7].
Most tubal mesosalpinx cysts are small in size and have no obvious clinical symptoms. Painful symptoms occur only when the cyst becomes larger and compresses the abdominal organs and tissues, but complications such as hemorrhage, torsion, or rupture are also rare [6]. When the diameter of the cyst is larger than 5 cm, the weight of the distal end of the fallopian tube increases, and the center of gravity changes, which may lead to torsion of the mesangial root and/or ovary [8, 9]. Blockage of the blood supply artery can cause venous reflux obstruction, and in severe cases, it may cause ischemic necrosis of the ipsilateral fallopian tubes and ovaries [3]. Tubal mesosalpinx cysts in adolescent females and pregnant women tend to increase suddenly in size. It has been suggested that it may be due to the elevated hormone levels in adolescent females and pregnant women, which cause increased secretion of epithelial cells within the cysts. Therefore, the accumulation of secretions within the cyst leads to an increase in its volume, and it easily merges with the self-torsion or accessory torsion of the cyst [10, 11]. In this paper, both girls experienced tubal mesosalpinx cysts with adnexal torsion shortly after menarche, which may also be related to increased hormone levels leading to cyst enlargement, consistent with the above literature.
Tubal mesosalpinx cysts are mostly benign, while junctional or malignant cysts are rare. They usually present as unilocular cystic lesions with thin smooth walls. If there is a papillary protrusion inside the cyst that is larger than 5 cm, the risk of malignancy increases [6, 12].
The fact that it is challenging to diagnose paratubal and parovarian cysts. Multiple studies have shown that only 30–44% of paratubal tube cysts are accurately diagnosed preoperatively [3, 13, 14]. Ultrasound is the preferred examination for detecting adnexal masses. If torsion is suspected, a color Doppler examination should be added [13]. Tubal mesosalpinx cysts are often located on one side of the adnexal region or next to the uterorectal fossa. When the cyst is larger, it may be located in the anterior upper part of one side of the uterus, appearing circular or elliptical. The wall of the capsule is mostly thin and smooth, and the capsule is characterized by anechoic liquid dark areas. There may be divisions within the cystic mass, and when combined with bleeding, weak echoes of small light spots can be observed inside the cyst, even presenting as a cystic solid or as a fluid-filled plane. If combined with tubal torsion, a thickened, twisted, and locally dilated anechoic tubular structure can be seen next to the cyst, and the torsion may display a “vortex sign”. The dilated tubes are located on the inner side of the affected ovary and gradually become thinner towards both ends, forming " beak signs” [3, 6, 15, 16]. If further ovarian torsion occurs, it will manifest as significant enlargement of the affected ovary, enhanced or reduced echogenicity, and disappearance of blood flow signals within the ovary. It should be noted that the presence of blood flow signals in the ovary does not exclude the possibility of torsion [13]. However, when the boundary between the mesosalpinx cyst and surrounding tissues is unclear, ultrasound is prone to missing diagnosis. The “ovarian crescent sign(OCS)” is a marker used in ultrasound to identify the nature of adnexal masses. This phenomenon is that normal ovarian tissue can be seen next to the adnexal mass, which is of great value for preoperative differentiation of benign or malignant adnexal masses. It can help to exclude invasive ovarian malignant tumors to some extent [5, 17, 18]. We reviewed the ultrasound images of two patients in this study and found the presence of OCS. Unfortunately, the primary diagnosis doctor, due to the lack of experience and specialized training on how to evaluate OCS, did not accurately identify this sign. In the second case, ultrasound revealed a large cystic mass in the right adnexal region pulling the ovary secondary to torsion, and an enlarged ischemic right ovary was detected next to the torsion tip. This patient was diagnosed by ultrasound with concomitant accessory torsion.
CT manifestations of mesosalpinx cysts are mainly circular or quasi-circular cystic masses near the uterus, with a few resembling sausages or serpentine cystic shadows. Cysts are often solitary and thin-walled with smooth margins and localized thickening of the cyst wall on enhancement scans. The capsule has a homogeneous water density with no enhancement; the density may increase when infection or bleeding occurs. The typical sign of tubal mesosalpinx cysts is the " holding ball” sign of the broad ligament of the uterus. When the cyst is large, it can compress and displace the abdominal organs. The larger the cyst, the more prone it is to pedicle torsion and rotation around the vascular pedicle axis. The most direct sign is the thickening and twisting of the fallopian tubes. Multiplanar reconstruction is particularly helpful for assessing the relative positions of the ovary and uterus, with the uterus typically pulled toward the side of torsion [3, 6, 19]. In addition, CT can help rule out other causes of lower abdominal pain, such as appendicitis [13]. In this report, both CT scans revealed cystic masses in the pelvic cavity, but the origin of the masses was difficult to determine and it was difficult to distinguish on imaging whether the masses originated from the ovary, fallopian tubes, or mesosalpinx.
MRI, with its advantages of high soft-tissue resolution, and multidirectional and multisequence imaging, can detect smaller lesions that are insensitive to ultrasound and can initially determine the benign or malignant nature of the lesions. Tubal mesosalpinx cysts on MRI mainly appear as round or round-like cystic lesions with a watery signal that is low on T1WI and high on T2WI. After enhanced scanning, the cyst wall shows enhancement, but there is no enhancement inside the cyst [20]. Compared with ultrasound and CT, MRI can more clearly display signs such as dilated tubes, beak signs, and twisted pedicles [8]. Especially if the patient is obese and the cyst is large, it is difficult for the ultrasound to determine its position relative to the ovary. In this case, MRI compensates for the shortcomings of ultrasound with a larger field of view showing the location of the cyst to the ovary, and it is also easier to show the relative positions of the uterus and ovary, with the uterus shifted to the side of the abnormality in the event of torsion [3, 21]. Moreover, if there is no enhancement of the ovary on MRI enhancement scans, it is strongly suspected that torsion has caused ischemic necrosis of the ovary. In the first patient of this report, preoperative MRI revealed the enlarged ovary and upward flipping of the adnexa, which ultrasound failed to clearly show. MR can compensate for missed ultrasound findings. Unfortunately, the second patient did not undergo MR examination.
The main imaging features of adnexal torsion include twisted and thickened fallopian tubes, accompanied by ovarian enlargement and displacement, and pulling of the uterus to move towards the affected ovary side [3, 22, 23]. In this paper, the preoperative MRI of the first case showed enlarged ovaries with upward flipping of the adnexa. The second case showed the thickened and twisted fallopian tube. The lower edge of the large cyst pulled the ovary and the right horn of the uterus, causing deformation and displacement of the ovary, and pulling the uterus towards the twisted side. Both cases in this paper were adnexal torsion due to tubal mesosalpinx cysts, with the tubal thickening and torsion being more pronounced.
Diseases predisposing to adnexal torsion include hydrosalpinx, paratubal cysts, ovarian teratomas, and cysts [8, 13]. Preoperative imaging to identify ovarian and tubal mesosalpinx cysts is challenging. When complications such as torsion or rupture occur, a clear diagnosis is rare before surgery, and surgery and pathology are required to make a clear diagnosis. In addition, the torsion of the hematosalpinx in patients with Mayer-Rokitanskt-Kuster-Hauser (MRKH) Syndrome is rare but still possible [24]. Therefore, adolescents with adnexal torsion should be aware of the presence of MRKH syndrome.
Conclusion
Tubal mesosalpinx cysts combined with adnexal torsion are rare acute abdominal conditions, and improving the accuracy of preoperative imaging diagnosis is crucial. MRI, as a supplement to ultrasound and CT, provides a broader field of view and effective information, aiding in comprehensive diagnosis and treatment, and reducing adverse outcomes. Imaging examinations should be timely, convenient, and precise, facilitating rapid diagnosis and guiding treatment to avoid delays. Nonetheless, laparoscopic exploration remains the gold standard for diagnosis and treatment. Immediate surgery can prevent damage to the ovaries and fallopian tubes, preserving reproductive function.
Data availability
Data is provided within the manuscript.
References
Zvizdic Z, Bukvic M, Murtezic S, Skenderi F, Vranic S. Giant Paratubal Serous Cystadenoma in an adolescent female: Case Report and Literature Review. J Pediatr Adolesc Gynecol. 2020;33(4):438–40. https://doi.org/10.1016/j.jpag.2020.03.010
Alpendre F, Pedrosa I, Silva R, Batista S, Tapadinhas P. Giant paratubal cyst presenting as adnexal torsion: a case report. Case Rep Womens Health. 2020;27:e00222. https://doi.org/10.1016/j.crwh.2020.e00222
Dawood MT, Naik M, Bharwani N, Sudderuddin SA, Rockall AG, Stewart VR. Adnexal Torsion: review of Radiologic appearances. Radiographics. 2021;41(2):609–24. https://doi.org/10.1148/rg.2021200118
Barloon TJ, Brown BP, Abu-Yousef MM, Warnock NG. Paraovarian and paratubal cysts: preoperative diagnosis using transabdominal and transvaginal sonography. J Clin Ultrasound. 1996;24(3):117–22. https://doi.org/10.1002/(SICI)1097-0096(199603)24:3%3C;117::AID-JCU2%3E;3.0.CO;2-K
Hillaby K, Aslam N, Salim R, Lawrence A, Raju KS, Jurkovic D. The value of detection of normal ovarian tissue (the ‘ovarian crescent sign’) in the differential diagnosis of adnexal masses. Ultrasound Obstet Gynecol. 2004;23(1):63–7. https://doi.org/10.1002/uog.946
Kiseli M, Caglar GS, Cengiz SD, Karadag D, Yılmaz MB. Clinical diagnosis and complications of paratubal cysts: review of the literature and report of uncommon presentations. Arch Gynecol Obstet. 2012;285(6):1563–9. https://doi.org/10.1007/s00404-012-2304-8
Gupta A, Gupta P, Manaktala U, Khurana N. Clinical, radiological, and histopathological analysis of paraovarian cysts. J -Life Health. 2016;7(2):78. https://doi.org/10.4103/0976-7800.185337
Qian L, Wang X, Li D, Li S, Ding J. Isolated fallopian tube torsion with paraovarian cysts: a case report and literature review. BMC Womens Health. 2021;21(1):345. https://doi.org/10.1186/s12905-021-01483-2
Breitowicz B, Wiebe BM, Rudnicki M. Torsion of bilateral paramesonephric cysts in young girls: Torsion of bilateral paramesonephric cysts. Acta Obstet Gynecol Scand. 2005;84(2):199–200. https://doi.org/10.1111/j.0001-6349.2005.0255c.x
Muolokwu E, Sanchez J, Bercaw JL, et al. Paratubal cysts, obesity, and hyperandrogenism. J Pediatr Surg. 2011;46(11):2164–7. https://doi.org/10.1016/j.jpedsurg.2011.07.011
Devouassoux-Shisheboran M, Silver SA, Tavassoli FA. Wolffian adnexal tumor, so-called female adnexal tumor of probable wolffian origin (FATWO). Hum Pathol. 1999;30(7):856–63. https://doi.org/10.1016/S0046-8177(99)90148-X
Thanasa A, Thanasa E, Xydias EM, et al. Pueperal Paratubal Cyst Torsion and secondary fallopian tube torsion without ovarian involvement: a Case Report. Cureus Published Online March. 2023;22. https://doi.org/10.7759/cureus.36540
Thakore SS, Chun MJ, Fitzpatrick K. Recurrent ovarian torsion due to Paratubal cysts in an adolescent female. J Pediatr Adolesc Gynecol. 2012;25(4):e85–7. https://doi.org/10.1016/j.jpag.2011.10.012
Darwish AM, Amin AF, Mohammad SA. Laparoscopic management of paratubal and paraovarian cysts. JSLS. 2003;7(2):101–6.
Gross M, Blumstein SL, Chow LC. Isolated fallopian tube torsion: a rare twist on a common theme. Am J Roentgenol. 2005;185(6):1590–2. https://doi.org/10.2214/AJR.04.1646
Narayanan S, Bandarkar A, Bulas DI. Fallopian tube torsion in the Pediatric Age Group: radiologic evaluation. J Ultrasound Med. 2014;33(9):1697–704. https://doi.org/10.7863/ultra.33.9.1697
Stankovic ZB, Bjelica A, Djukic MK, Savic D. Value of ultrasonographic detection of normal ovarian tissue in the differential diagnosis of adnexal masses in pediatric patients. Ultrasound Obstet Gynecol. 2010;36(1):88–92. https://doi.org/10.1002/uog.7557
Van Holsbeke C, Van Belle V, Leone FPG, et al. Prospective external validation of the ‘ovarian crescent sign’ as a single ultrasound parameter to distinguish between benign and malignant adnexal pathology. Ultrasound Obstet Gynecol. 2010;36(1):81–7. https://doi.org/10.1002/uog.7625
Low S, Ong C, Lam S, Beh S. Paratubal cyst complicated by tubo-ovarian torsion: computed tomography features. Australas Radiol. 2005;49(2):136–9. https://doi.org/10.1111/j.1440-1673.2005.01405.x
Kishimoto K, Ito K, Awaya H, Matsunaga N, Outwater EK, Siegelman ES. Paraovarian cyst: MR imaging features. Abdom Imaging. 2002;27(6):685–9. https://doi.org/10.1007/s00261-002-0014-6
Stefanopol IA, Baroiu L, Neagu AI, et al. Clinical, imaging, histological and Surgical aspects regarding Giant Paraovarian cysts: a systematic review. Ther Clin Risk Manag. 2022;18:513–22. https://doi.org/10.2147/TCRM.S361476
Rha SE, Byun JY, Jung SE, et al. CT and MR Imaging features of Adnexal Torsion. Radiographics. 2002;22(2):283–94. https://doi.org/10.1148/radiographics.22.2.g02mr02283
Jung SI, Park HS, Yim Y, et al. Added Value of using a CT coronal reformation to diagnose Adnexal Torsion. Korean J Radiol. 2015;16(4):835. https://doi.org/10.3348/kjr.2015.16.4.835
Naem A, Sleiman Z. Unusual torsion of Hematosalpinx in a case of MRKH Syndrome. J Minim Invasive Gynecol. 2023;30(2):85–6. https://doi.org/10.1016/j.jmig.2022.11.010
Funding
No funding.
Author information
Authors and Affiliations
Contributions
J.C. contributed to the investigation, data curation, and writing the original draft; C.L. contributed to preparing and image analysis; H.Z. contributed to surgical management and revising the work; D.L. contributed to the investigation and data curation; and W.W. contributed to the conceptualization, methodology, validation, reviewing and editing the article, and project administration. All the authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This is not applicable, as this is a case report.
Consent for publication
Informed consent was obtained from the patient’s parents for publication of clinical information and photographs. The parents of the two patients have signed the written informed consent forms.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, J., Li, C., Zhang, H. et al. Tubal mesosalpinx cysts combined with adnexal torsion in adolescents: a report of two cases and review of the literature. BMC Pediatr 24, 525 (2024). https://doi.org/10.1186/s12887-024-05001-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-024-05001-9