- Case Report
- Open access
- Published:
Unusual presentation of miliary tuberculosis in a 12-year-old girl: a case report
BMC Pediatrics volume 24, Article number: 223 (2024)
Abstract
Background
Miliary tuberculosis (TB) is a lethal hematogenous spread form of mycobacterium tuberculosis with approximately 15–20% mortality rate in children. The present report highlights the clinical manifestations of an unusual presentation of miliary tuberculosis in a 12-year-old girl.
Case presentation
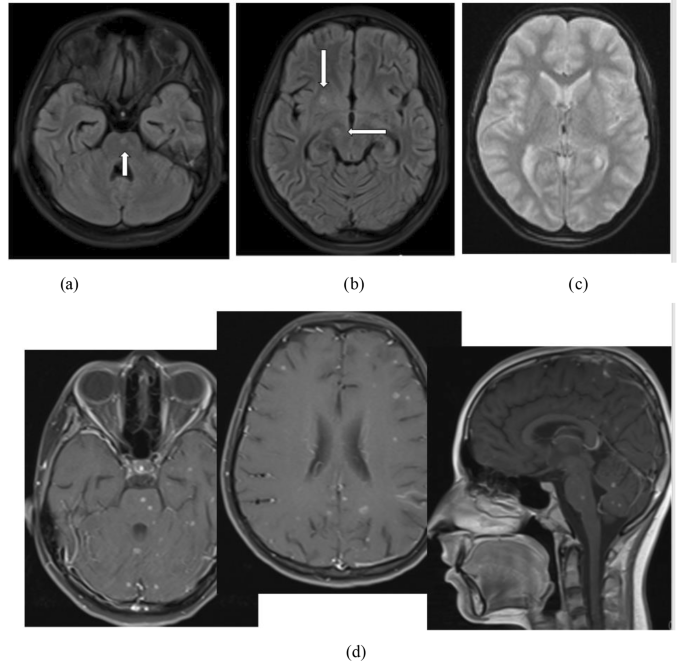
In this case, extensive lung involvement was presented despite the absence of respiratory symptoms. Also, some central hypo-intense with hyper-intense rim nodules were detected in the brain’s pons, right cerebral peduncles and lentiform nucleus.
Conclusion
The results of this study showed that severe miliary TB may occur even in a person who received the Bacille Calmette-Guérin (BCG) vaccine.
Background
Tuberculosis (TB), caused by mycobacteria, is a preventable and curable disease with 1.5 million mortality annually most of them live in low and middle-income countries [1]. Intracranial tuberculosis (ITB) is an unusual and rare presentation of extrapulmonary tuberculosis [2]. The incidence of ITB is 5–30% of all intracranial lesions [3]. Nevertheless, it often remains underestimated [4]. Disseminated TB and miliary TB had similar pathogenesis but the anatomical-pathological findings are different [5]. Disseminated TB is an important cause of mortality and morbidity in children under 15 years old especially in developing countries [6]. Disseminated TB describing as entering the bacteria into the systemic circulation, then they multiply and infect extrapulmonary organs [7]. They account for highly variable clinical manifestations including fever, weight loss, anorexia and nocturnal sweating [8]. Miliary TB is a lethal hematogenous spread form of mycobacterium tuberculosis to several organs, diagnosed by the presence of a diffuse miliary infiltrate on a chest X-ray, CT scan and pathological evidence [9]. Peripheral lymphadenopathy and hepatosplenomegaly are the most common childhood military TB signs. The mortality rate of childhood miliary TB is approximately 15–20% [10, 11]. As a huge challenge, the nonspecific clinical features of miliary TB often result in delayed diagnosis followed by a poor prognosis condition [12]. Also, this clinically silent TB leads to inadequate treatment in young children [13]. So, in children, considering ITB as a differential diagnosis is important. The present case report highlights the clinical presentation of unusual miliary TB evidence in a 12 years old girl.
Case presentation
A 12-year-old girl was admitted to a general hospital, in one of the western cities of Mazandaran province, with chief complaints of muscle atonia, and foam coming from the mouth for 20 s following fever and transient left hemiparesis. Ten minutes later, she agitated and presented generalized tonic-clonic movements lasting for 15 min and decreased consciousness following urinary incontinence. During this episode, she didn’t have foam coming from her mouth. She was intubated immediately and transferred to the PICU (Pediatric intensive care unit) of a tertiary hospital, in Sari, Mazandaran province. She had been visited by a general physician due to fever (T = 38.5 oc), vomiting (digested food particles and non-bloody), diplopia and headache one week before hospitalization and received symptomatic treatment. With relative recovery, the signs and symptoms aggravated the night before hospital admission. Her family reported unintentional weight loss accompanying anorexia and weakness from two months ago, but additional imaging was not performed.
Medical history and physical examination were as follows: The initial vital signs were blood pressure: 105/70 mmHg, the pulse rate: 110 beats per minute, respiratory rate: 22 per minute, axillary temperature: 37.4 oc and SPO2: 98% (intubated). Skin: Negative in terms of petechia, purpura and ecchymosis. Eyes: pale conjunctiva. Extremities: 1 + deep tendon reflexes. The tone and power of muscle were normal and there were not any signs of cerebellar or basal ganglion involvement. Lymph node: No lymphadenopathy. Chest and lung: No chest deformity, she was intubated, and symmetric lung sounds. Abdomen: No distention and organomegaly. No sign and symptom of increased intracranial pressure. She had no history of contact with Coronavirus disease 2019 (COVID-19) patients, contaminated water, rice field and trauma. She had fainted in her childhood period following excessive activity (medical follow-up showed cardiac chamber defect) and improved spontaneously when she was 3 years old. She completed all doses of recommended childhood vaccines but did not receive the COVID-19 vaccine. She had a drug allergy to Cefixime and penicillin and a food allergy to eggplant. Initially, her family did not report a positive family history of TB, but after the final diagnosis, they declared that her uncle died following TB 3 years ago.
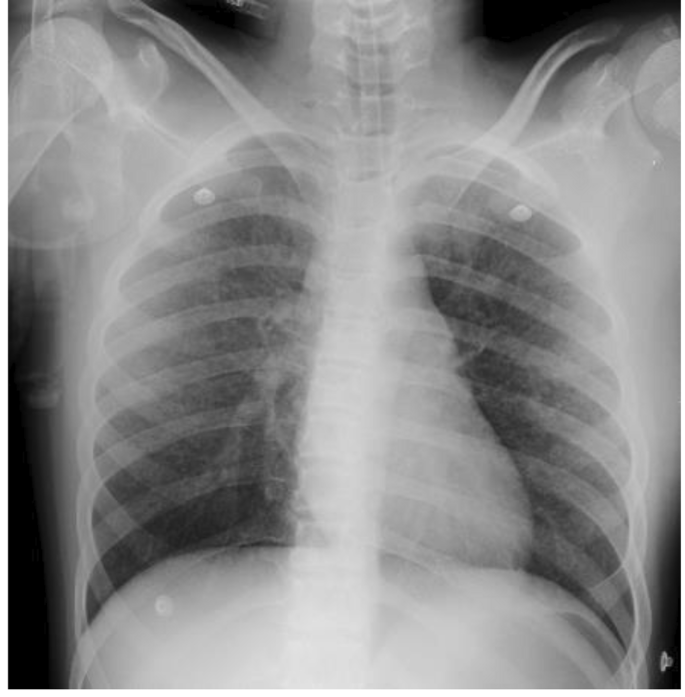
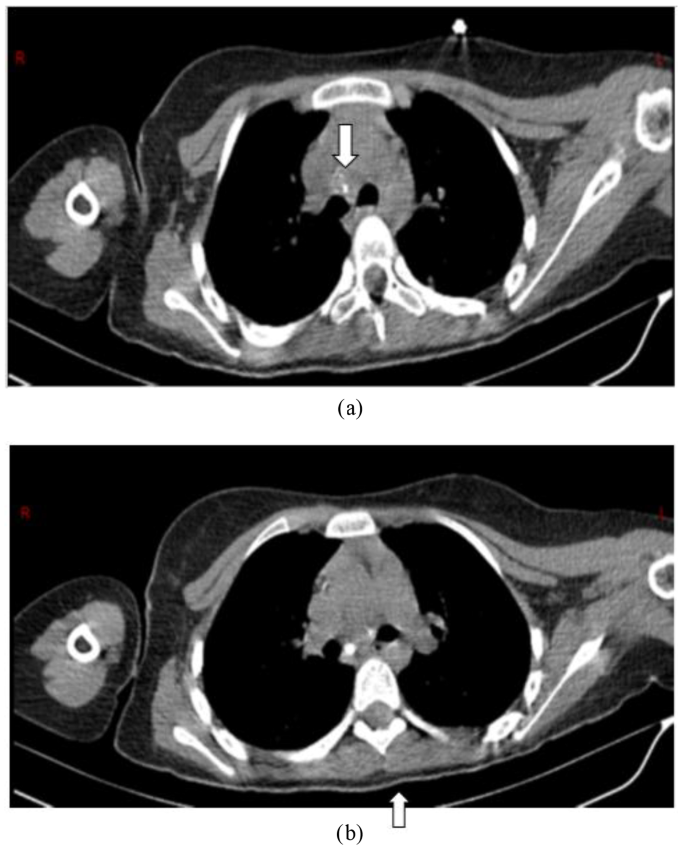
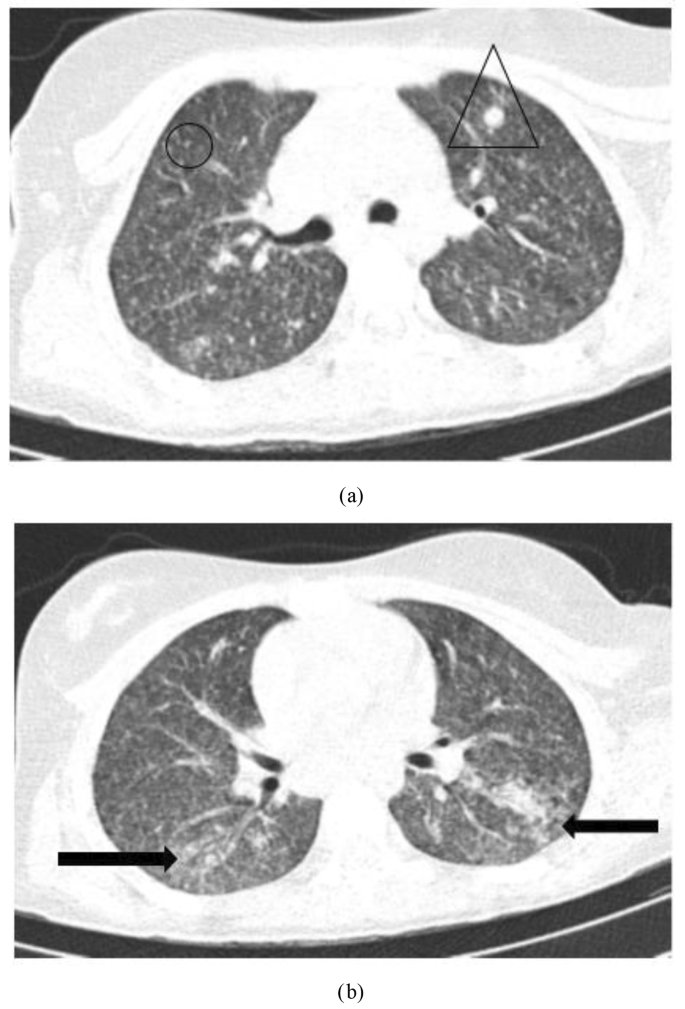
Para-clinical investigations: The result of COVID-19 Reverse transcription polymerase chain reaction (RT-PCR) and galactomannan level was negative. Also, the levels of HIV (human immunodeficiency virus) antibody, Venereal disease research laboratory (VDRL), CD4 (cluster of differentiation 4), CD19 and Complement hemolysis (CH50) were normal. The echocardiography showed mild Tricuspid valve regurgitation and mild pulmonary valve insufficiency. Also, there was no pulmonary hypertension. Based on the possible COVID-19 bilateral involvement in chest X-ray and lung CT scan, Pro-BNP, D-dimer and troponin levels were requested. Only the D-dimer level was high. It was 1710. The lumbar puncture (LP) was done on the first day of the PICU admission. The Cerebrospinal fluid (CSF) analysis results are presented in Table 1. Although, the girl had no signs and symptoms of meningitis including Brudzinski’s and Kernig’s signs, there was CSF involvement. CSF analysis showed increased levels of protein and WBC. The patient had not the coughing or sputum, so the gastric aspirate culture PCR (three times) had been done and the result was positive for miliary TB. Findings of the chest X-ray (Fig. 1), lung CT scan (Figs. 2 and 3) and brain MRI (Fig. 4) were suggestive of caseating tuberculomas. Finally, the miliary TB was diagnosed based on brain MRI, positive gastric aspirate culture and also two organs involvement. AP chest x-ray demonstrates wide spread tiny nodular opacities distributed throughout both lungs. The PPD test were normal.
A pediatric infectious diseases specialist prescribed rifampin, ethambutol, pyrazinamide, isoniazid and vitamin B6 (For prevention of the side effect of isoniazid) based on the miliary TB evidence in MRI. The anti-tuberculosis medication dosage was adjusted due to elevated AST and ALT levels 10 days later. So, the rifampin and isoniazid were discontinued and in the follow-up due to the normal levels of AST and ALT, the rifampin and isoniazid were added to the medication regimen. At the time of discharge, approximately one month later, the gastric aspiration result was negative. She was discharged in stable condition with fixed-dose combination anti-TB medication (III), acid folic and vitamin B6 tablets daily. On her follow-up, AST and ALT levels were normal. Also, her medication changed to two-drug formulations. The girl had been follow-up for at least one year and the MRI finding and gastric aspirate on follow-up were normal.
Brain MRI without contrast: 4-a & 4-b) Flair sequence: some central hypo-intense with hyper-intense rim nodules in the pons, right cerebral peduncles and lentiform nucleus (white arrows). 4-c) DWI/ADC: no restricted diffusion. 4-d) Contrast–enhanced MRI: Diffuse Multiple rim-enhancing nodules in both cerebral, cerebellar hemispheres and brainstem. These findings are suggestive of caseating tuberculomas with tuberculous meningitis. DWI: Diffusion-weighted imaging – ADC: Apparent diffusion coefficient
Discussion
In the present case report, the miliary TB evidence was presented in a 12 years old girl. Miliary TB has been more prevalent in middle age and older people than children [14, 15]. Also, 60% of the cases are male with a mean age of 55 years in studies [16,17,18]. Although the mean age of miliary TB patients has increased, the rates remain relatively low in children [19, 20]. In the present study, the unusual miliary TB pattern was seen in a 12 years old girl. The miliary TB in young patients is reported in TB-endemic countries [21]. Based on the results of a retrospective descriptive study in South Africa, 32.7% of children were TB meningitis. Also, the recent study reported 43.3% of children drug resistant was the main reason for hospitalization [22]. But, in our case, the girl had no drug resistance. Approximately 13% of the TB cases suffer from HIV infections [23]. TB becomes more generalized and affects more than one organ when progressive immunosuppression occurs [24]. However, the present case didn’t have HIV infection as co-infection or other immunodeficiency condition. Corticosteroid therapy can reactivate cryptic TB [25]. Song et al. reported a 36-year-old man who underwent corticosteroid therapy and two weeks later, he experienced an acute exacerbation of miliary TB [26]. But in our study, the patient had no history of recent corticosteroid therapy. Considering increased the number of BCG-vaccinated children and improving the diet status of children, we see the modified clinical profile of neurotuberculosis including TB meningitis nowadays with wide varieties of clinical manifestations according to the site of the brain lesion [27]. The clinical presentation of neurotuberculosis may be nonspecific leading to delayed treatment and poor clinical outcome [28]. The present case had diffuse multiple rim-enhancing nodules in both cerebral, cerebellar hemispheres and brainstem in the brain. The brain and central nervous systems are two target organs of mycobacterium tuberculosis that cause serious and dangerous forms of extrapulmonary tuberculosis [29]. The most obvious initial clinical symptoms of our case were fever, weight loss, anorexia and seizure. Other studies reported fever, cough, seizure, diarrhea, hepatomegaly, splenomegaly, jaundice, anorexia and weight loss as the most common clinical presentations in children [6, 30, 31]. A male three-months Brazilian infant was admitted with nocturnal fever, sweating and coughing 10 days before hospitalization and he was not responsive to antibiotic therapy. The results of the chest X-ray showed bilateral miliary TB and also CNS TB based on the CT-scan report [32]. Similar to our case, the recent case showed early diagnosis and treatment in endemic areas. Delayed diagnosis in miliary TB patients can cause serious complications including cranial nerve involvement, convulsions and death [16] as a seizure occurred in our case. Machida et al.’s report showed 1% of TB patients had CNS involvement which is about a high mortality rate and permanent neurological sequelae [33]. Fortunately, in the present case, follow-up interventions showed no neurological sequelae and she was in good general condition. Multiple diagnostic tests are provided to detect miliary TB, including PCR, sputum smear and acid-fast staining, in addition to histopathological findings but radiology plays a major role in this regard [34]. In this case, despite the absence of respiratory symptoms and non-significant lung involvement in chest X-ray, extensive lung involvement was seen including diffuse multiple miliary nodules. Also, a chest CT scan revealed some scattered micronodules in a random distribution in both lungs associated with patchy consolidation in lower lobes in favor of pulmonary TB. Additionally, in the brain, some central hypo-intense with hyper-intense rim nodules in the pons, right cerebral peduncles and lentiform nucleus, multiple diffuse rims enhancing nodules in both cerebral, cerebellar hemispheres and brainstem were obvious.
The COVID-19 pandemic has emerged new conditions, including neuro-COVID which has presented by lung involvement and seizure [35]. During the COVID-19 pandemic, miliary TB should be considered in TB endemic areas due to neuro-COVID diagnosis.
Our study showed that teenage patients might present extensive lung involvement in favor of miliary TB even in the absence of respiratory symptoms. Also, we found that severe miliary TB may occur even in a person who received the bacille Calmette-Guérin (BCG) vaccine. In an Iranian study, in 15 children aged under 72 months, disseminated BCG infection occurred after BCG vaccination [36]. Also, in patients with CNS symptoms including seizure especially in TB endemic areas, miliary TB should be considered as a differential diagnosis, to prevent delay in diagnosis and treatment. We live in the TB endemic area. So, when a patient is admitted with a decreased level of consciousness and there is no reasonable cause, we should consider TB as a differential diagnosis. In the current case report, due to early diagnosis and treatment, neurological sequelae were not observed.
Data Availability
Due to the privacy of the patients, the data generated during the current study are not publicly available but are available from the corresponding author upon reasonable request.
References
WHO. Health topics:Tuberculosis 2022 [updated 2020. Available from: https://www.who.int/health-topics/tuberculosis#tab=tab_1.
Frioui S, Jemni S. Cerebral tuberculoma: an entity not to ignore. Pan Afr Med J. 2016;24(1).
Zahrou F, Elallouchi Y, Ghannane H, Benali SA, Aniba K. Diagnosis and management of intracranial tuberculomas: about 2 cases and a review of the literature. Pan Afr Med J. 2019;34.
Alharbi A, Khairy S, Al Sufiani F, Alkhani A. Intracranial tuberculomas: a case report of clinical, radiological, and pathological characteristics. Int J Surg Case Rep. 2021;88:106477.
Buonsenso D, Mariani F, Morello R, Song R. State-of-the-art of miliary Tuberculosis in children: protocol for a scoping review of the literature. F1000Research. 2023;12(309):309.
Khan FY. Review of literature on disseminated Tuberculosis with emphasis on the focused diagnostic workup. J Fam Commun Med. 2019;26(2):83.
Krishnan N, Robertson BD, Thwaites G. The mechanisms and consequences of the extra-pulmonary dissemination of Mycobacterium tuberculosis. Tuberculosis. 2010;90(6):361–6.
Khan FY, Dosa K, Fuad A, Ibrahim W, Alaini A, Osman L, et al. Disseminated Tuberculosis among adult patients admitted to Hamad general hospital, Qatar: a five year hospital based study. Mycobact Dis. 2016;6(212):104172.
Sharma SK, Mohan A. Miliary tuberculosis. Tuberculosis and nontuberculous mycobacterial infections. 2021:415 – 35.
Starke JR. Tuberculosis in infants and children. Tuberculosis and nontuberculous mycobacterial infections. 2021:456 – 75.
Triasih R, Helmi R, Laksanawati IS. Clinical profile and outcome of extrapulmonary Tuberculosis in children in Indonesia. Pediatr Respirol Crit Care Med. 2018;2(3):51.
Letchuman V, Guillotte AR, Lundy PA, Dharia A, Lakis NS, Camarata PJ. Intracranial tuberculoma: a rare complication of extrapulmonary Tuberculosis. Illustrative case. J Neurosurgery: Case Lessons. 2022;4(1).
Abuhamed M, Bo X, Yan C. Central nervous system tuberculomas: a review article. Am J Infect Dis. 2008;4(2):168–73.
Lee J, Lim JK, Kim EJ, Lee DH, Kim YK, Yoo SS, et al. Comparison of clinical manifestations and treatment outcome according to age groups in adult patients with miliary Tuberculosis. J Thorac Disease. 2018;10(5):2881.
Munt PW. Miliary Tuberculosis in the chemotherapy era: with a clinical review in 69 American adults. Medicine. 1972;51(2):139–55.
Hosseini MJ, IMANI FA. Miliary tuberculosis with empyema, a case report. 2010.
Takahashi K, Akatsuka M, Yamamoto S. Miliary Tuberculosis complicated with acute respiratory distress syndrome and hemophagocytic syndrome. Oxf Med Case Rep. 2022;2022(1):omab142.
Arfaoui H, Aidou S, Bahma H, Jabri H, El Khattabi W, Afif H. Miliary Tuberculosis: Moroccan series of 101 cases. SAS J Med. 2022;2:100–5.
Sahn SA, Neff TA. Miliary Tuberculosis. Am J Med. 1974;56(4):495–505.
Kilgore J, Pelletier J, Becken B, Kenny S, Das S, Parnell L. Miliary Tuberculosis in a paediatric patient with psoriasis. BMJ Case Reports CP. 2021;14(3):e237580.
organization WH, Tuberculosis, WHO. ; 2021 [Available from: https://www.who.int/health-topics/tuberculosis#tab=tab_1.
Musonda H, Rose P, Switala J, Schaaf H. Paediatric admissions to a TB hospital: reasons for admission, clinical profile and outcomes. Int J Tuberc Lung Dis. 2022;26(3):217–23.
Pinzon RT, Wijaya VO, Paramitha D. Encephalitis due to miliary Tuberculosis in a patient with human immunodeficiency virus: a case report. J Clin Tuberculosis Other Mycobact Dis. 2021;23:100230.
Letang E, Ellis J, Naidoo K, Casas EC, Sánchez P, Hassan-Moosa R, et al. Tuberculosis-HIV co-infection: progress and challenges after two decades of global antiretroviral treatment roll-out. Arch Bronconeumol. 2020;56(7):446–54.
Sahn SA, Lakshminarayan S. Tuberculosis after corticosteroid therapy. Br J Dis Chest. 1976;70:195–205.
Song M, Kim SJ, Yoo JY. Corticosteroid-induced exacerbation of cryptic miliary Tuberculosis to acute respiratory distress syndrome: a case report. Medicine. 2020;99:46.
Yeredla VVR, Tammali S, Ravula CJ, Kalivela S. Changing trends in the clinical profile of childhood in Tuberculosis patients-at a tertiary centre. EUREKA: Health Sciences. 2023;2:24–32.
de Gusmão Filho FA, Marques HHdS, Marques-Dias MJ, Ramos SRS. Tuberculose do sistema nervoso central em crianças: 1. Apresentação clínica E Laboratorial. Arq Neuropsiquiatr. 2001;59:71–6.
Babamahmoodi F, Alikhani A, Yazdani Charati J, Ghovvati A, Ahangarkani F, Delavarian L et al. Clinical epidemiology and paraclinical findings in tuberculosis patients in north of Iran. BioMed research international. 2015;2015.
Tanrikulu C, Gürkan F, DAĞLI CE, Ayfer G, Süner A. A comparative review of pediatric and adult patients with miliary Tuberculosis. Eur J Gen Med. 2007;4(2).
Gurkan F, Bosnak M, Dikici B, Bosnak V, Yaramis A, Tas MA, et al. Miliary Tuberculosis in children: a clinical review. Scand J Infect Dis. 1998;30(4):359–62.
de Andrade MR, Lacerda CA, Vicente JFC, Lamounier JA. An infant with central nervous system tuberculosis and miliary tuberculosis.
Machida M, Toyoda K, Matsuda M, Sumida K, Yamamoto A, Sakurai K, et al. Extensive perivascular dissemination of cerebral miliary tuberculomas: a case report and review of the literature. Acta Radiol Open. 2018;7(12):2058460118817918.
Mortazavi-Moghaddam SGR, Sharifzadeh GR, Rezvani MR. Status of exudative pleural effusion in adults of South Khorasan Province, northeast Iran: pleural Tuberculosis tending toward elderly. Iran J Med Sci. 2016;41(4):322.
Frontera J, Mainali S, Fink EL, Robertson CL, Schober M, Ziai W, et al. Global consortium study of neurological dysfunction in COVID-19 (GCS-NeuroCOVID): study design and rationale. Neurocrit Care. 2020;33(1):25–34.
Rezai MS, Khotaei G, Mamishi S, Kheirkhah M, Parvaneh N. Disseminated bacillus Calmette–Guerin Infection after BCG vaccination. J Trop Pediatr. 2008;54(6):413–6.
Acknowledgements
The authors would like to extend their gratitude to all the healthcare providers who were involved in the treatment of the present case.
Funding
None.
Author information
Authors and Affiliations
Contributions
MR: critically edited the manuscript. MK: Drafting the manuscript. MN, AA, AH, MS, MR: Involved in treatment. FG: Interpreting the CXR, MRI and CT-scan. All authors approved final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research objectives were explained to the subjects, and they were ensured of confidentiality terms regarding their personal information.
Consent for publication
Informed consent for publication was obtained from patient’s legal guardian.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kamali, M., Navaeifar, M.R., Abbaskhanian, A. et al. Unusual presentation of miliary tuberculosis in a 12-year-old girl: a case report. BMC Pediatr 24, 223 (2024). https://doi.org/10.1186/s12887-023-04427-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-023-04427-x